Breast reconstruction is a challenging aspect of plastic and reconstructive surgery. Mastectomy reconstruction involves re-creating the breast when skin is thin and devitalized and or radiated from the mastectomy surgery. When a breast implant becomes exposed after mastectomy reconstruction the patient and surgeon are faced with a challenging problem. The implant can become exposed from poor quality of the mastectomy skin, previous radiation, recent chemotherapy, poor nutrition, or a combination of multiple factors.

It is helpful prior to embarking on an immediate reconstruction of the situation at hand to reverse any of the factors that are contributing to the implant exposure. If the factors cannot be optimized, then it may be best to remove the implant and delay the reconstruction for a future time when the factors are optimized. Alternatively, a partial reconstruction immediately to stabilize the soft tissues can be undertaken to maximize successful placement of an implant six months to one year after the soft tissues are stabilized.
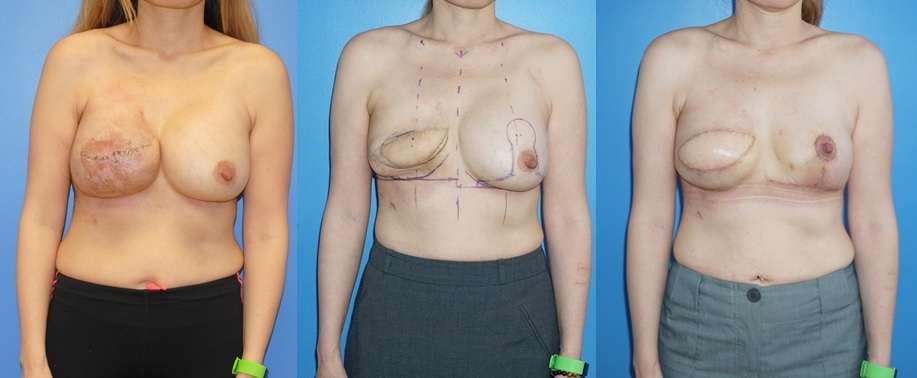
When the mastectomy skin is thin, devascularized, and of poor quality, the skin and soft tissue can be augmented or replaced with autologous tissue. The latissimus dorsi flap is a very versatile flap that can be harvested and transferred from the back to the anterior aspect of the chest to replace some of the skin. It is helpful for the physician and patient to have the discussion that the reconstructive process can often take several operations and several months to correct the problem.

The first step in the reconstructive process is to remove any foreign material that can be safely removed and then transfer the autologous tissue from the back to the chest. When the autologous tissue is transferred from the back to the chest, the remaining mastectomy skin will contract around the cavity where the implant was located. This contraction process is even more exaggerated when the skin has been previously radiated.
Once the soft tissue has stabilized and is ready for an implant to be placed, it is helpful to choose the smallest implant that the patient can be happy with. This will help minimize future complications such as capsular contracture and bottoming out. These complications are two very different phenomena that can occur in this group of patients post-operatively. Downsizing the previous implant size in the affected breast will also necessitate downsizing in the contralateral breast. This often requires a mastopexy reduction pattern to facilitate symmetry as the radiated breast can often be higher and more contracted than the non-radiated side.
When the implant has been placed on the reconstructed side, there will be additional changes to the position of the implant over the course of a year. The reconstructed side may still have a weak inframammary fold with resulting bottoming out or simply a new position of the inframammary fold after placement of a mammary prosthesis. Re-suspension of the fold can be undertaken at the one-year mark. Bottoming out of the mammary prosthesis can again be prevented with downsizing of the implant to prevent the weight of the implant descending to a lower position on the chest wall.
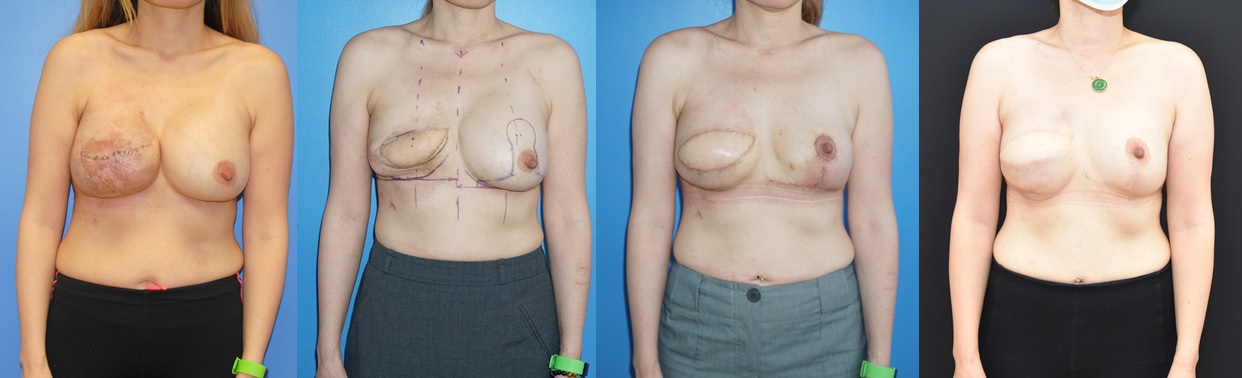
Once a new equilibrium of the mammary prosthesis has been reached, the infra-mammary fold can be re-created and a smaller, higher profile implant cam be placed to produce the same breast projection. Occasionally, the contralateral mammary prosthesis of the non-reconstructed breast can be removed to minimize variables associated with two implants and possibly make the reconstruction simpler.
On the autologous reconstructed side, one reason for bottoming out may be redundant autologous skin that is no longer needed. The additional skin that remains on the skin paddle can be removed either partially or entirely. If only a portion of the skin paddle is to remain, the skin paddle can be deepithelialized to retain as much autologous volume to the reconstructed breast as possible.

The reconstructive process can take several steps and operations to create a reasonable reconstructed breast mound. Before each procedure and for six weeks after it is important for patients to consume 1-2 grams of protein per kg of body weight per day. The healing from the reconstructive procedures consumes a significant amount of energy in healing. It is important to have the proper nutritional to facilitate healing.

